CGM for People Without Diabetes
Oct 25, 2024
With Abbott's recent launch of Lingo, the first FDA-approved over-the-counter wellness Continuous Glucose Monitor (CGM) in the U.S., the conversation around CGMs for people without diabetes has gained significant attention.
While CGMs like Lingo resemble traditional devices like FreeStyle Libre, they now come with wellness-focused apps to help users "reduce glucose spikes and improve overall health".
Get Access To Updated Diabetes Technology Courses
But it's not just Abbott!
More and more companies are marketing CGMs to the general public:

Their claims?
These monitors can:
- Help make healthier decisions and prevent diabetes
- Aid in weight loss and reduce hunger
- Improve sleep, mood, and energy
- & Boost sports performance
But are these claims backed by solid science, or are they more marketing hype?
Let's explore the pros and cons of CGMs for people without diabetes.
- What Are Normal Glucose Values for People Without Diabetes?
- How Many Glucose Spikes Can You Expect?
- What Causes Glucose Spikes?
- How Bad Are Glucose Spikes for Your Health?
- What about Glucose Dips?
- Risks of Using CGMs in People Without Diabetes
- Benefits of CGMs in People Without Diabetes
- How to use CGMs in people without diabetes
- Future directions
- Conclusion
1. What Are Normal Glucose Values?
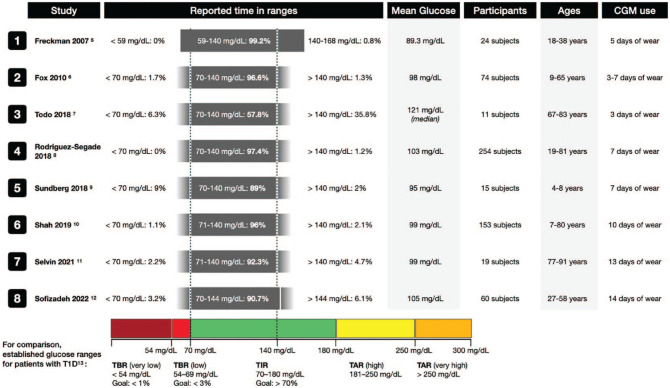
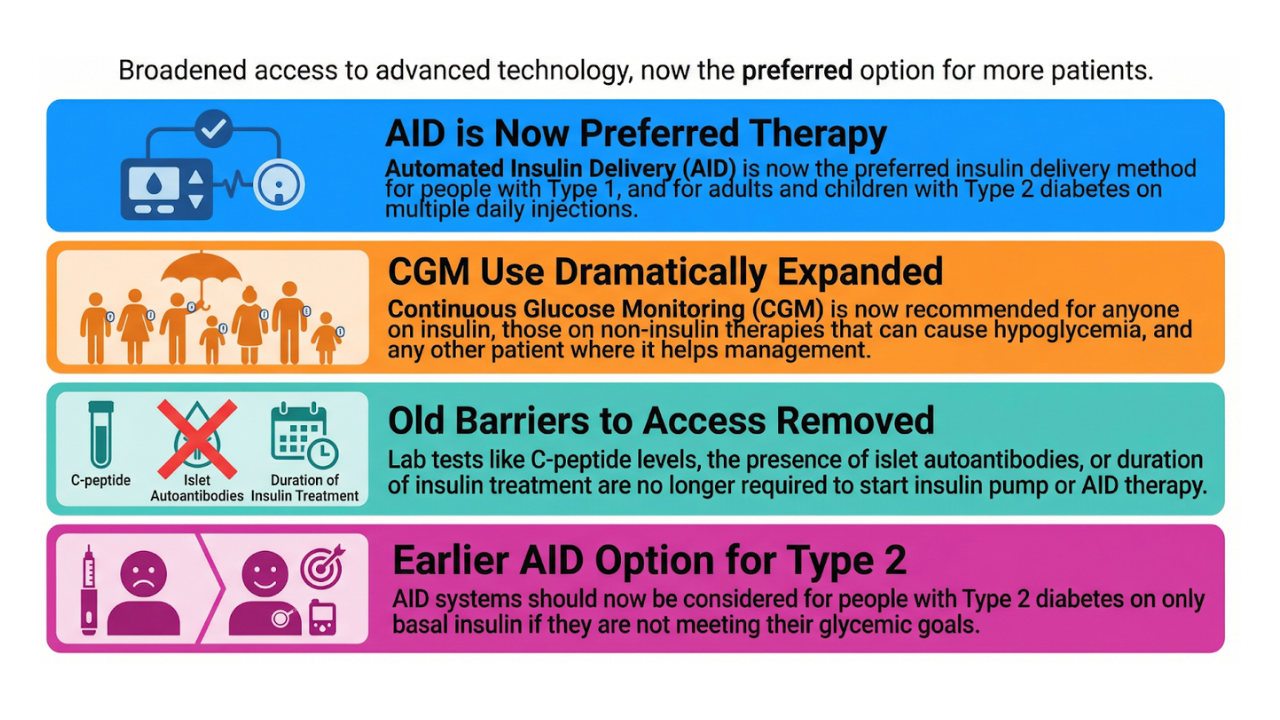
Picture > Klonoff et al. JDST 2023
Research indicates that most individuals without (pre)diabetes have sensor glucose values between 70 and 140 mg/dL (3.9 and 7.8 mmol/L) for more than 95% of the time.
This means that even among individuals with a normal glucose metabolism, glucose levels occasionally fall outside this range.
👉 Time spent between 70–140 mg/dL (3.9-7.8 mmol/L): Over 95% of the time.
👉 Glucose spikes and dips: Approximately 5% or 75 minutes per day may be spent either:
- Above 140 mg/dL (7.8 mmol/L)—glucose spikes.
- Below 70 mg/dL (3.9 mmol/L)—glucose dips.
2. How Many Glucose Spikes Can You Expect?

Glucose spikes in people without diabetes can be quantified by the duration of time spent above 140 mg/dL (7.8 mmol/L), the number of spikes experienced or the glycemic variability.
👉 Time above 140 mg/dL (7.8 mmol/L):
- Varies from 30 minutes to 3 hours per day depending on the population studied.
👉 Incidence of glucose spikes:
- In a study with 254 adults who used an iPro2 CGM for 5 days, 73% experienced at least one glucose spike >140 mg/dL (7.8 mmol/L).
- In a study with 104 adults who used a FreeStyle Libre for 7 days, 52% experienced at least one glucose spike >180 mg/dL (10 mmol/L).
👉 Glycemic variability:
As individuals transition from healthy to prediabetic or diabetic states, overall glycemic variability tends to increase.
Note: There's a notable decrease in the "mobility" of the glucose signal—the extent of glucose fluctuations relative to overall variability. This suggests that not all types of glucose variability are detrimental. Similar to heart rate variability, the ability to promptly correct changes in glucose levels might be a positive sign.
3. What Causes Glucose Spikes?

Picture > Zheevi et al. Cell 2015
Although 42 factors have been identified that affect glucose levels, the most important cause of glucose spikes is carbohydrates.
Postprandial Glucose Response (PGR):
- Simply put, the more sugar or carbs in your food, the more dramatic the spike in your glucose levels can be. But it's not just about quantity—the type of carbs matters too.
- Here's where it gets interesting: your glycemic response is highly individualized.
- For example, a banana or a cookie might cause a significant spike in one person but have minimal effect on another.
Factors Influencing the Postprandial Glucose Response (PGR):
👉 Timing of Eating:
- Breakfast leads to a higher PGR than lunch and dinner.
- Earlier dinner times and shorter eating windows reduce glycemic variability.
👉 Meal Composition:
- Adding protein, fat, and fiber lowers PGR.
👉 Previous Meals:
- Skipping breakfast can lead to a higher PGR at lunch.
- A high-protein breakfast can reduce PGR at lunch.
- Carb and fiber snacks can reduce PGR at dinner.
👉 Exercise Routine:
- Post-meal exercise reduces PGR by around 50%, for example 1000 steps or “soleus push-ups” while seated.
- Less sedentary behavior and more physical activity lead to less glycemic variability.
- High-intensity exercise can increase insulin sensitivity for up to 3 days post-exercise.
👉 Sleep Quality:
- Poor sleep efficiency, later bedtime routines and chronic sleep debt are associated with higher PGR.
👉 Stress Levels:
- Acute stress can lead to glucose spikes and delay the decrease of PGR.
- Stress might delay the decrease of the PGR, although this effect was more clear in people with diabetes.
Differences in Glycemic Variability and Glucotypes:

Picture > Hall et al. PLoS Biol 2018
People without diabetes can experience significant differences in how their glucose levels fluctuate—a concept known as glycemic variability.
These differences are so distinct that researchers have identified different "glucotypes," or patterns of glucose regulation unique to each person.
This means that two people might eat the same meals but have entirely different glucose responses due to their individual glucotype.
Additional Factors Influencing Glycemic Variability:
👉 Age: Decline in insulin sensitivity and secretion with age.
👉 Gender: Slight differences in PGR between men and women.
👉 Genetics: Certain genes linked to higher insulin resistance.
👉 BMI: Both underweight and overweight individuals have higher glycemic variability.
👉 Depression: Patients with more severe depressive symptoms had higher glycemic variability.
👉 Gut Microbiome: PGR related to microbiome activity.
By understanding these factors, you can gain insights into how your lifestyle choices affect your glucose levels.
Recognizing that your responses may be unique to you empowers you to make informed decisions to manage glucose spikes more effectively.
4. How Bad Are Glucose Spikes for Your Health?
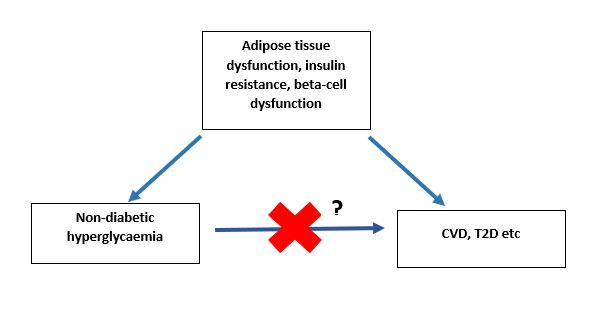
Picture > Dr Guess’s Bog 2023
The clinical significance of postprandial glucose spikes is a topic of ongoing debate.
👉 Potential risks of glucose spikes:
- Glucose spikes seem to be the first sign of beta-cell dysfunction and progression toward diabetes.
- A high glucose variability is associated with worse cognitive functions, diabetes, cardiovascular complications and mortality.
👉 Lack of Definitive Proof:
- There is no definitive evidence that glucose spikes directly cause diabetes or cardiovascular disease.
- Glucose spikes might just be a symptom of an underlying metabolic problem.
Consequently, it remains uncertain whether reducing glucose spikes can prevent diabetes or other metabolic conditions.
For now, there is no research proving that controlling or reducing glucose spikes directly improves the health of people without diabetes.
5. What about Glucose Dips?
Picture > Presentation dr. Tracey McLaughlin @DTM2024
Although people without diabetes spend a minimal time below 70 mg/dL (3.9 mmol/L), hypoglycemic events can occur.
Incidence of Glucose Dips
- In a study with 153 people using a Dexcom G6 sensor for 10 days, 28% experienced at least one event <54 mg/dL (3.0 mmol/L).
- In another study with 254 participants using an iPro CGM for 5 days, 44% experienced at least one event <70 mg/dL (3.9 mmol/L).
Causes of Glucose Dips
- False lows: Some of the glucose dips might be false as CGMs are less accurate at the lower glucose values.
- Compression lows: Some glucose dips are causes by lying on the sensor, for example at night.
- Reactive hypoglycemia: If the hypoglycemic event haps 2-5 hours after food intake, they can be called a "reactive hypoglycemia".

Picture > Karen Kennedy Blog 2024
Clinical Significance of Glucose Dips
👉 Glucose values between 54–70 mg/dL (3.0–3.9 mmol/L) without complaints:
Most experts are not particularly concerned about glucose values between 54–70 mg/dL (3.0–3.9 mmol/L) in individuals not taking glucose-lowering medications,
especially if these events occur without symptoms (such as hunger, anxiety, dizziness and sweating).
👉 Glucose values between 54–70 mg/dL (3.0–3.9 mmol/L) with complaints or <50 mg/dl (<3.0 mmol/L):
The clinical significance of this reactive hypoglycemia is not entirely clear.
- Some evidence suggests that postprandial glucose dips can predict appetite and energy intake in healthy individuals.
- However, other research did not find an increased appetite during glucose dips.
While definitive claims cannot be made, preventing symptomatic postprandial "reactive hypoglycemia", by choosing lower glycemic foods to reduce glucose spikes, could theoretically help to prevent these glucose dips and the possible accompanying hunger after meals ("hangry" feeling).
6. Risks of Using CGMs in People Without Diabetes
#1. Anxiety Over Glucose Dips
Frequent indications of hypoglycemia can contribute to:
- Anxiety Disorders and Mental Burden: Increased stress and worry about health.
- Sleep Disturbances: Nighttime alarms may cause sleep deprivation, affecting overall health.
- Increased Healthcare Costs: More frequent contact with healthcare providers.
- Unnecessary Eating: Consuming food when not necessary to correct perceived low glucose levels, potentially leading to weight gain.
💡 Pro-tip:
- Educate users about possible low readings.
- Reassure that events between 54–70 mg/dL (3.0-3.9 mmol/L) without symptoms are generally not worrisome.
- Provide access to a blood glucose meter for verification.
#2. Anxiety Over Glucose Spikes
Occasional glucose spikes can cause:
- Health Concerns and Anxiety: Worrying about glucose spikes.
- Obsessive Behavior & Development of Eating Disorders: Over-focusing on CGM data and food intake can lead to orthorexia or other restrictive eating patterns.
- Eliminating foods perceived to cause spikes may result in food avoidance, unhealthy weight loss, and reduced quality of life.
💡Pro-tip:
- Set Appropriate Goals: For example a time between 70-140 mg/dl (3.9-7.8 mmol/L) of > 90% for people without diabetes.
- Emphasize that occasional glucose spikes and dips are normal and may not indicate a health issue.
#3. Unhealthy eating behaviours

Picture adapted from presentation dr. Richard Bergenstal @EASD2024
Misconceptions about glucose spikes may lead individuals to avoid healthy activities
- Avoiding Complex Carbohydrates: leading to imbalanced nutrition
- Avoiding Exercise: because normal glucose increases during physical activity might be interpreted as negative
- High-Fat Diets: because believing that any meal not causing a spike is healthy, potentially increasing intake of unhealthy fats.
💡Pro-tip:
- Understand / Educate that not all glucose spikes are harmful, and that not all foods that don't cause glucose spikes are healthy.
- Reducing spikes should involve healthy behaviors.
- Ideally people seek help from a dietician to make the right choices.
#4 Costs
CGMs are not reimbursed for people without diabetes.
Costs can be approximately $45–$150 per sensor, or $100 per month.
💡Pro-tip:
- Use CGMs intermittently to reduce costs. You can already learn a lot by wearing just 1 CGM.
- Focus on proven strategies like diet and exercise. Supplements like Zoe Daily30+ or Anti-Spike Formula are not backed by solid scientific evidence.
#5 Skin Reactions
Skin irritation and itching are common with CGM use.
Although very rare, some individuals might develop a contact allergy to a specific CGM.
💡Pro-tip:
- Apply lipid ointments on the skin after removal of the CGM.
- In people who have skin reactions: replace the use of alcohol wipes by a barrier spray or cream.
- If severe irritation or allergy occurs, consider switching sensor types.
7. Benefits of CGMs in People Without Diabetes

Picture > Presentation dr. Tracey McLaughlin @DTM2024
#1 Diagnostic: Early Detection of (Pre)Diabetes
Although CGM metrics should not be used for diagnosing (pre)diabetes, they can be a trigger to go to your physician.
- When to go to your physician: If your time >140 mg/dL (>7.8 mmol/L) is >10%, it's best to do a venous blood draw (fasting glucose or HbA1c) to rule out (pre)diabetes.
- Adapt report settings: If you're using a normal FreeStyle Libre or Dexcom sensor, you can adapt the report settings of your readout software to 70-140 mg/dl (3.9-7.8 mmol/L).
- Do not use GMI: For those without diabetes, the Glucose Management Indicator (GMI)—an estimated HbA1c from CGM reports—is not sufficiently accurate for drawing conclusions.
#2 Therapeutic: Guiding Lifestyle Modification & Personal Nutrition
👉 CGM can help to eat healthier and exercise more.
Having access to real-time glucose data can encourage individuals to choose healthier foods, engage in regular physical activity, and monitor the effects of their lifestyle choices on their glucose levels.
These healthier choices can lead to less mortality and prevention of type 2 diabetes.
- Several studies have shown that an optimal diet has a significant effect on mortality (Fadnes et al. Nature Food 2023, Shan et al. JAMA 2023, Vinke et al. Diabetes Care 2021)
- Lifestyle changes aimed at weight reduction, optimised diet and exercise, can help to prevent diabetes.
- Research supports that these lifestyle interventions can reduce the incidence of type 2 diabetes by about 58% in high-risk individuals.
👉 CGM can also help to lose weight
- Although there is no evidence that a low-glycemic diet is better than any other well-balanced low-caloric diet, it is a valid option for people who aim to lose weight.
- The addition of a CGM provides usable data for both immediate intervention (for example postprandial exercise to decrease glucose spikes), as well as retrospective dietary evaluation.
Important Consideration:
- Reducing glucose spikes leads to weight loss only if healthy behaviors are adopted.
- Strategies like exercising, eating more vegetables, and adding fibers and protein are effective.
- Switching to saturated fats or avoiding exercise-induced glucose spikes is not helpful.
👉 Potential benefits on Sleep, Energy and Mood
Although there is not enough evidence to make any medical claims, some individuals might experience that stabilising their glucose patterns helps for better sleep, energy levels and mood.
👉 CGMs are used a lot by atletes

Picture > Presentation dr. Howard Zisser @DTM2024
A lot of elite atletes use CGMs to understand their glucose metabolism and performance during and after endurance exercises, although there is no evidence for a certain "peak performance range".
- First of all, it’s important to note that CGMs are less accurate during exercise.
- It is usually recommended to avoid (reactive) hypoglycemia during exercise as this might hinder performance, although hypoglycemia during exercise happens frequently and is not always symptomatic, and that not all feelings of hypoglycemia are caused by glucose dips.
- Contradictory, some athletes experience higher blood glucose levels.
#4 Curiosity & Metabolic Awareness
Although the benefits of CGMs in people without diabetes are highly debated, they are used also by people who are just curious about how their body reacts to different foods.
It can make you "metabolically aware" and can can give you some insights in the carb content of our day-to-day nutrition.
These learnings of wearing a CGM are especially interesting for medical students and healthcare providers.
In conclusion there is no consensus on the benefits of CGMs in people without diabetes.
- Most physicians are awaiting data before recommending CGM to people without diabetes, although some physicians are advocating use of CGM to prevent type 2 diabetes and improve overall health - partially based on the idea that absence of proof is not proof of absence.
- There are also more and more dieticians who recommend CGMs as a motivational tool and to track the diet of their patients.
- Some individuals are choosing to self-pay for CGMs, especially the ones who are into longevity, self-optimisation and prevention.
8. How to use CGMs in people without diabetes

Understand normal values
- Normal Values: If you don't have diabetes, you can expect your glucose values to be 70-140 mg/dl (3.9-7.8 mmol/l) 95% of the time. That means that 5-10% of the time or 75-150 minutes per day you will experience glucose spikes >140 mg/dl (7.8 mmol/L) and glucose dips (<70 mg/dl or 3.9 mmol/L). This considered to be normal.
- When to go to your physician: If your time >140 mg/dl (>7.8 mmol/L) is >10%, it's a good idea to go to a physician to rule out prediabetes.
- Goals for Prediabetes: If you have prediabetes, it has been recommended to strive for a time between 54-140 mg/dl (3.0-7.8 mmol/l) of > 95%.
- Reassurance around glucose dips: Glucose dips 54-70 mg/dl (3.0-3.9 mmol/L) without symptoms are not considered as worrysome if you are not using glucose-lowering medications.
- Accuracy: CGMs are not always accurate (especially not on the first day). If you are worried about a glucose spike or glucose dip, you can verify it with a finger prick test.
Learn what lifestyle choices affect your glucose levels
- Monitor Frequently: Look at your CGM glucose reading often during the day. The more you look, the more you learn. See what you can learn about how your meals and beverages impact your glucose.
- Identify Triggers: If you notice a glucose spike, be curious and think what could have caused this spike: food, exercise, stress... - Some sensor apps include glucose spike detection and offer a way to log your meals, exercise and stress level.
- Experiment: If you see a glucose spike after a certain food amount/type, use couterfactional thinking and try out a different food and check if the postprandial glucos response is better.
Tips to reduce glucose spikes and dips:
- Choose Low-Glycemic Foods: Opt for foods with a lower glycemic load (= lower portion of carbs and low-glycemic index) to avoid sharp spikes. A dietitian can offer personalized advice on this.
- Pair Carbs with Fibre, Protein or Fat: This can help slow down the absorption of glucose, leading to more stable blood sugar levels.
- Eat Carbs Last: Some people suggest to eat your protein and non-starchy vegetables first, and the carbs on your plate last.
- Increase Physical Activity: Regular exercise is an effective way to lower overall glucose levels and improve your body's ability to manage blood sugar.
- Strive for a healthy BMI: If your BMI is >25, losing weight can ameliorate your insulin sensitivity, which will reduce your baseline and postprandial glucose levels.
Conclusion
In some people without diabetes, wearing a CGM can give you insights in and motivate you to do healthy behaviour.
Be aware that lowering glucose spikes and “stabilising your glucose” might be beneficial, but it is not proven that this will make you “healthier”.
So above all, do what you feel most comfortable with.
9. Future directions
Holistic approach
Instead of solely focusing on glucose, we see that digital therapeutics (apps) are focusing on several behavioral changes to improve metabolic health.

Picture > Presentation dr. Tracey McLaughlin @DTM2024
Integration with Wearables
Integration of lifestyle information can be used for glucose optimization.
To make it easier, several apps are connecting to more wearables such as activity trackers, sleep trackers, and heart rate monitors.

Picture > Presentation dr. Michael P. Snyder @DTM2024
Automatic Meal Tracking
Carb counting can be made easier by using food pictures and large language models.
CGM data can also predict the other macronutrients that have been eaten.

Picture > Presentation dr. David Kerr @DTM2024
Artificial Intelligence and Subphenotyping
Artificial intelligence is being used to subfenotype an individual based on their postprandial glucose response.

Picture > Presentation dr. Michael P. Snyder @DTM2024
Personalised Lifestyle Intervention
On top of personalised nutrition, metabolic subfenotyping can lead to personalised behaviour recommendations or lifestyle intervention.
For example:
- people who are more insulin resistent might benefit more from exercising in the morning,
- while people who are more insulin sensitive might bnefit more from exercising in the afternoon.

Picture > Presentation dr. Michael P. Snyder @DTM2024
10. Conclusion
CGMs are not officially recommended for people without diabetes, but their use in this group is growing rapidly.
While we can't yet make definitive medical claims, CGMs could theoretically serve as valuable motivational tools for promoting healthy habits like better nutrition and regular exercise.
We encourage more research into CGM use among people without diabetes, focusing not just on improving accuracy but also on understanding what constitutes normal glucose levels in this population. It's crucial to explore how these levels relate to the risk of developing other health conditions.
As big data and AI continue to evolve, we anticipate gaining better insights into which patterns of glycemic variation are beneficial and how personalized lifestyle recommendations can enhance health.
These findings are likely to benefit a large number of people, not just those with diabetes, making CGMs a valuable tool for promoting better health and longevity.
Interested in Learning More?
If you're curious about how CGMs work and whether they might be right for you or your patients, consider exploring our courses on CGMs.
We offer a free, accredited general course, as well as device-specific courses on the most popular CGMs available today.
Kind regards,